What Causes the Pulp Of the Tooth to Become Infected?

Throbbing tooth pain or sensitivity when you take a sip of coffee or enjoy some ice cream could be more than an inconvenience. These and other symptoms might be signs of infected tooth pulp. So what causes this issue, and what can your dentist do to address it? Learn all about infected tooth pulp symptoms and diagnosis below.
What Is the Pulp?
Pulp is a gelatinous organic material composed of connective tissue, nerves, artery and vein that occupies the tooth’s center in a hollow cavity called the pulp chamber. The pulp is the “heart” of the tooth, providing blood to the tooth’s root.
The tooth’s pulp is surrounded immediately by dentin, which comprises the largest part of the tooth. Enamel, the hardest substance in the body, is the thin outer covering of the tooth that protects the dentin and the pulp. The pulp produces new dentin and gives the tooth sensation from heat, cold, sweetness and pressure. The protection of this part of our tooth is crucial.
However, several things can broach the pulp chamber and damage the pulp:
- Caries, or deep cavities
- Fractures
- Deep cracks that cause the tooth pulp to become exposed
- Trauma from a fall or blow
- Periodontal disease
- Bruxism, or grinding one’s teeth
What Is Pulpitis?
Reversible Pulpitis
Reversible pulpitis causes inflammation only, as the pulp chamber is still unbreached. Your tooth’s pulp may have been overstimulated by:
- A cavity
- A broken filling
- A cracked or chipped tooth
- Extra wear on the teeth, caused by a malocclusion, such as an underbite or crossbite
- Bruxism
The most easily recognized symptom of reversible pulpitis is tooth pain, especially throbbing pain in sync with your heartbeat. However, since people frequently interpret other issues like allergies and sinus pressure as tooth pain, it is important to consider other symptoms, such as:
- Temperature and sweetness sensitivity: You may feel a brief, sharp pain when your affected tooth comes in contact with something hot, cold or sweet. The pain will only last a few seconds after that contact has ended.
- Inflammation: Tooth pulp inflammation can affect other areas of your mouth, and your gums around the affected tooth may be swollen and red.
- Pain from tapping or pressure: You may feel a sharp pain if you tap or apply pressure to the affected tooth.
Treatment for reversible pulpitis depends on its underlying cause. Whatever the issue, your dentist can quickly and non-invasively correct the problem.
Cavities are the most common cause of reversible pulpitis. In this case, the treatment is nearly identical to filling a cavity. Your dentist might use a bonded filling. You may receive a crown for a cracked tooth, or your dentist might order a nightguard or occlusal adjustment for bruxism or malocclusions. They may also prescribe antibiotics for any remaining infection or inflammation.
After treatment, the symptoms correct themselves in two to three days.
Irreversible Pulpitis
In irreversible pulpitis, the pulp chamber is breached. Bacteria cause pulp infection along with inflammation. The infected pulp can lead to tooth pain, inflammation and sensitivity, similar to reversible pulpitis. However, as irreversible pulpitis is a more severe condition, its symptoms are also more severe:
- Temperature and sweetness sensitivity: You may experience pain from exposure to heat, cold or sweets that lingers for more than 30 seconds after contact.
- Inflammation: Tooth pulp inflammation can cause swelling in your cheek or the gums at the top of the tooth.
- Increased pain: Tap or pressure tests will produce a stronger, sharper pain that may make eating and swallowing difficult. You may also experience persistent, intense throbbing pain without direct stimulus, and your pain may increase when you lie down.
- Persistent unpleasant taste: Infected tooth pulp may cause bad breath or a continual unpleasant taste in your mouth.
- Signs of infection: Symptoms of pulp infections include fever, chills and swollen glands. In cases of severe infection, you may also develop a painful rash.
- Trismus: Also known as lockjaw, trismus is difficulty opening your mouth.
This condition requires immediate attention. The pulp is dying, creating a condition called pulp necrosis. Necrosis of the pulp leads to gas and pus formation that produces swelling and pain — the classic toothache.
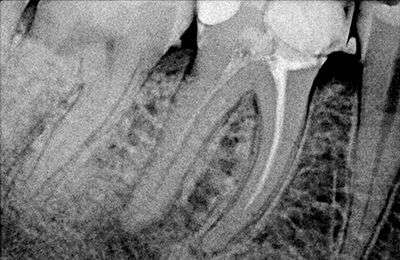
An endodontist — a dentist specializing in conditions affecting teeth interiors and roots — must decide whether to do root canal therapy to save the tooth or have the tooth extracted.
A root canal starts with the endodontist removing the dead pulp, debris and infection from your tooth’s interior and roots. Once they have removed the pulp infection, they fill each root’s canal with sealant and affix a crown. If the endodontist determines that your tooth must be extracted, you may choose to fill the space with a bridge or implant.
Endodontists often prescribe antibiotics and analgesic medications to accompany pulpitis-related root canals and extractions.
How Do We Diagnose Pulpitis?
Determining Symptoms
- How long has your tooth been bothering you?
- Where does it hurt?
- Is your pain constant, or does it come and go? If it comes and goes, how frequent are your bouts of pain?
- If your pain comes and goes, how long does it last — a few seconds, minutes or longer?
- Does anything make the pain better or worse?
- Is the pain sharp or dull? Has it changed since it first began?
- Does it hurt only in one spot, or does it extend to other areas?
Clinical Exam and X-Rays
- Palpation and visual assessment: Gently rolling a finger over your gums helps the dentist evaluate any swelling in other areas and check for sensitivity to pressure over the bone.
- Tapping test: The dentist taps the affected tooth and monitors your reaction to determine if you are experiencing any pain from inflammation.
- Hot and cold test: The dentist places hot and cold substances against the affected tooth to evaluate your response. Strong pain that disperses quickly is a sign of reversible pulpitis, while strong lingering pain indicates irreversible pulpitis. No response to a cold stimulus may indicate that the pulp is dead.
- Electric pulp test: This test can help confirm whether the pulp is still alive. The dentist applies a gradually increasing electrical current to the affected tooth and monitors your response.
What To Do When The Pulp Of The Tooth Is Exposed
- Sinusitis
- Meningitis
- Brain abscess
- Ludwig’s angina
- Pericarditis
Irreversible pulpitis can also lead to a dental abscess, which can cause cellulitis, a bacterial infection affecting the skin’s inner layers. Once cellulitis has set in, the bacteria can spread to the bone. This infection, known as osteomyelitis, often requires surgery to remove the infected bone.
Prevention of Pulpitis
Schedule a Root Canal Appointment Today
Schedule an Appointment for Your Root Canal at Midtown Endodontist NYC Today
BOOK AN APPOINTMENT
Treating your pulpitis now can save your tooth and safeguard your overall health. If you have a pulp infection, Midtown Endodontist NYC, the top endodontists in NYC is here to help.
Headed by the acclaimed Dr. Steven Lipner, our team is here to treat your toothache in the most gentle, conservative and efficient manner. If you have dental pain, we make it go away. Do not hesitate to call — we are here for you.
Contact us today at (646) 374-2569 to make an appointment for a free consultation.
 Our Providers
Our Providers
 Blog
Blog
 Contact us
Contact us
 Endodontics
Endodontics
 Root Canal Treatment
Root Canal Treatment
 Emergency Root Canal
Emergency Root Canal
 Root Canal Retreatment
Root Canal Retreatment
 Complimentary Teeth Whitening
Complimentary Teeth Whitening
 Teeth Whitening
Teeth Whitening




